Background
Life expectancy for individuals with sickle cell disease (SCD) has improved significantly in the last 50 years, creating a new population of older adults with SCD; however, life expectancy of adults with SCD is still up to 30 years shorter than African Americans in the general population and much lower than whites. SCD complications cause significant morbidity, requiring patients to make complex decisions about end of life care. Yet, there is a paucity of literature on SCD advance care planning (ACP), to guide providers on how to address ACP in this population. Thus, the purpose of this study was to assess barriers and facilitators to ACP for older adults with SCD.
Methods
We recruited 19 older adults with SCD (age > 50) from a comprehensive SCD center in the Southeastern United States. We conducted semi-structured interviews by phone or in person. Interview questions addressed aging with SCD, living beyond SCD life expectancy, experience with health care, experience with end of life care, comfort discussing death and end of life care, presence and nature of prior ACP discussions, and preferences for future ACP discussions. Audio-recorded interviews were transcribed verbatim. The data were analyzed using conventional content analysis.
Results
The mean age of participants was 57 years (range 50-71) and 47% (n = 9) were female. Most participants were diagnosed with SCD several years after birth and were told that they were not expected to live past age 18. Four of 19 participants had written advanced directives. Most participants were comfortable and willing to discuss ACP and thought that SCD ACP discussions should ideally start in early adulthood.
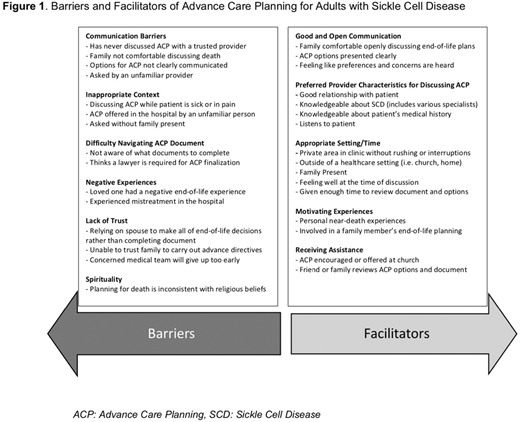
Barriers to ACP included lack of communication, inappropriate contexts for ACP discussions, lack of trust, difficulty navigating ACP documents, and spirituality (Figure 1). Lack of communication included limited to no communication from trusted healthcare providers about ACP preferences. Inappropriate contexts for ACP discussions included being approached at difficult times by unfamiliar providers, such as being asked to complete advance directives while sick in the hospital by a provider who did not know the patient well. Trust was a barrier, as several participants were concerned that being asked about ACP while sick meant providers were giving up on them; others were unsure if they could trust providers or family members to carry out their end of life wishes as written. They reported difficulty navigating ACP documents and several participants incorrectly assumed a lawyer was required to finalize ACP documents. Finally, spirituality was a barrier as some participants reported that end of life planning was inconsistent with their religious beliefs.
Facilitators of ACP included discussion at the right time, provider familiarity and knowledge, presence of family, and assistance in completing ACP documents. Participants expressed a desire to have an opportunity to openly communicate their end of life wishes with their provider when they were not sick in the hospital. They preferred discussing ACP with a provider whom they had a good relationship with, was familiar with their history, and they perceived was knowledgeable about SCD. Participants identified their SCD provider, PCP, or pulmonologist as suitable providers to talk to about ACP. Most preferred their family to be present during the ACP discussion. Those that had already completed advance directives at the time of the study received assistance from someone outside the health system to do so, such as help from their church, a lawyer, or their family.
Conclusion
Older adults with SCD expressed a desire for communication about ACP from trusted providers who are knowledgeable about SCD and want to have ACP conversations when they are feeling well. In addition, having the patient's family present and giving them assistance may increase the patient's comfort in completing their advance directives. The lack of communication from trusted providers or communication from unfamiliar providers about ACP during hospitalizations for acute complications are major barriers to creating advance directives for older adults with SCD. Future research is needed to obtain providers' perspectives on barriers to initiating conversations about ACP with adults with SCD. We will use these results to inform development of patient-centered and culturally-sensitive interventions to improve ACP in adults with SCD.
Strouse:Takeda: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.